
Business owners, executives and shift workers might think slight changes in their regular sleep patterns and duration make no difference to their overall night’s rest and recovery – but think again.
New research from Flinders University shows the chances of higher blood pressure increases exponentially, particularly for overweight middle-aged men, with every hour of sleep they lose or change to their regular nighttime routine.
A new study, published in the prestigious American Heart Association journal Hypertension, is one of the first large-scale extended studies into the effect of variable sleep patterns on blood pressure.
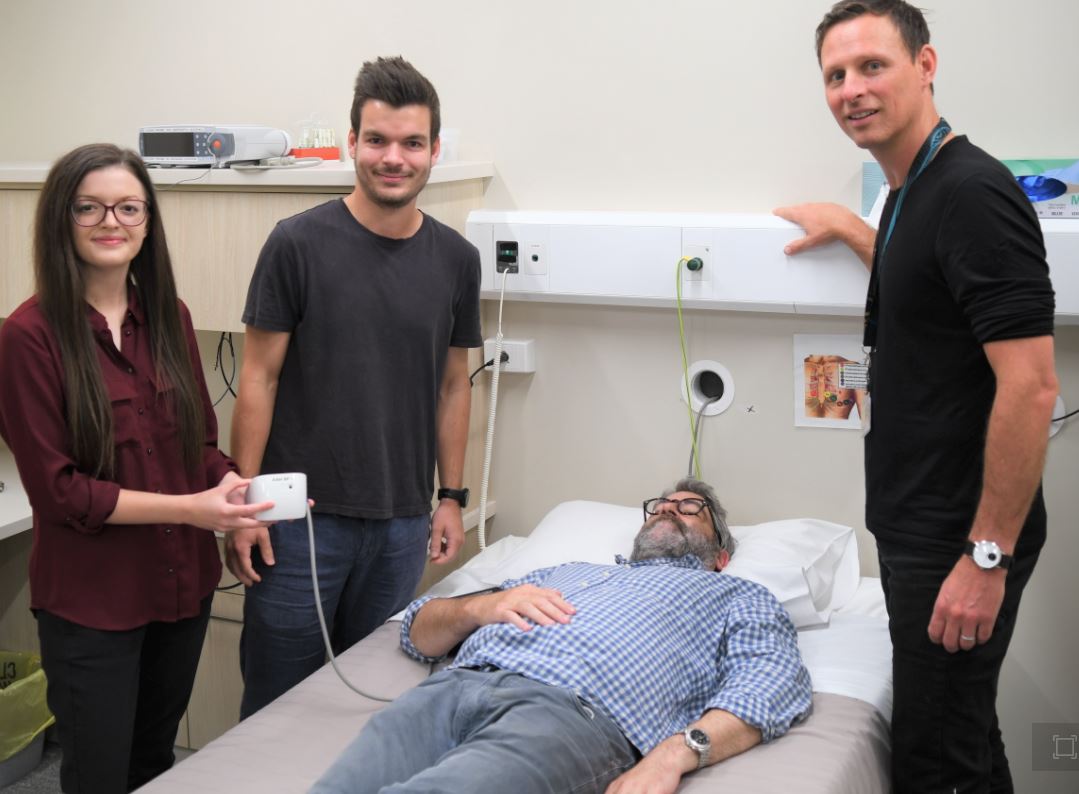
The study involved a global sample covering the equivalent of more than 2 million nights of home sleep data measured from 12,287 adults – 88% of them men and, on average, overweight (BMI; 28±6kg/m2) – in their own homes using portable under-mattress sensor monitoring technology and remote blood pressure assessment.
On average, each participant had 30 separate blood pressure recordings over the nine-month study timeframe.
The Australian and French research team found a strong correlation between elevated hypertension and irregular sleep duration and timing – emphasising the need for more awareness about the links between circadian control systems and health.
“Not only should we monitor the amount of sleep, but we should also keep our resting schedule as regular as possible,” says Flinders University sleep psychology researcher Dr Hannah Scott, a co-lead author of the new journal article.
Regularly varying nightly bedtimes by more than about 30 minutes was associated with a 32% increase in hypertension risk. Higher nightly variability in other timing measures – such as mid-sleep time and wake-up time – were associated with greater hypertension risk.
Given a complex interplay between sleep history, sleep need and circadian influences, irregular sleep can lead to further disruption and even more variation in sleep patterns, researchers warn.
As well, inadequate sleep (less than six hours) and even too much sleep (long sleep of nine or more hours) were also associated with increased blood pressure, similar to other studies.
“However, this study also shows that night-to-night variation in sleep timing and duration can have a similar effect, even if people get the recommended 7-9 hours on average for adults aged 18-65 years,” adds co-author Dr Bastien Lechat.
“These findings illustrate how irregularity in both duration and timing of sleep onset and waking up is a clear risk marker for poor cardiovascular health, along with the total number of hours we sleep,” says Dr Lechat.
“Further investigations may find other cardio and health issues are connected to day-to-day fluctuations in sleep duration and timing.”
Senior Flinders University sleep researcher Professor Danny Eckert says: “This study highlights another concept in establishing good sleep habits which are vital for physical and mental health, in particular the cardiovascular system.
“It adds to what we already know about poor sleep hygiene and higher risk of obesity, cardiovascular disease and hypertension in general.”
The article, ‘Sleep irregularity is associated with hypertension: Findings from over two million nights with a large global population sample’ (2023) by Hannah Scott, Bastien Lechat, Alisha Guyett, Amy Reynolds, Nicole Lovato, Ganesh Naik, Sarah Appleton, Robert Adams, Pierre Escourrou (Centre Interdisciplinaire du Sommeil, France), Peter Catcheside and Danny J Eckert has been published in the journal Hypertension DOI: 10.1161/HYPERTENSIONAHA.122.20513

