
A major new $1 million digital health project led by Flinders University will target the needs of people living with chronic disease in low socioeconomic neighbourhoods to build a robust model for other cities and regional areas.
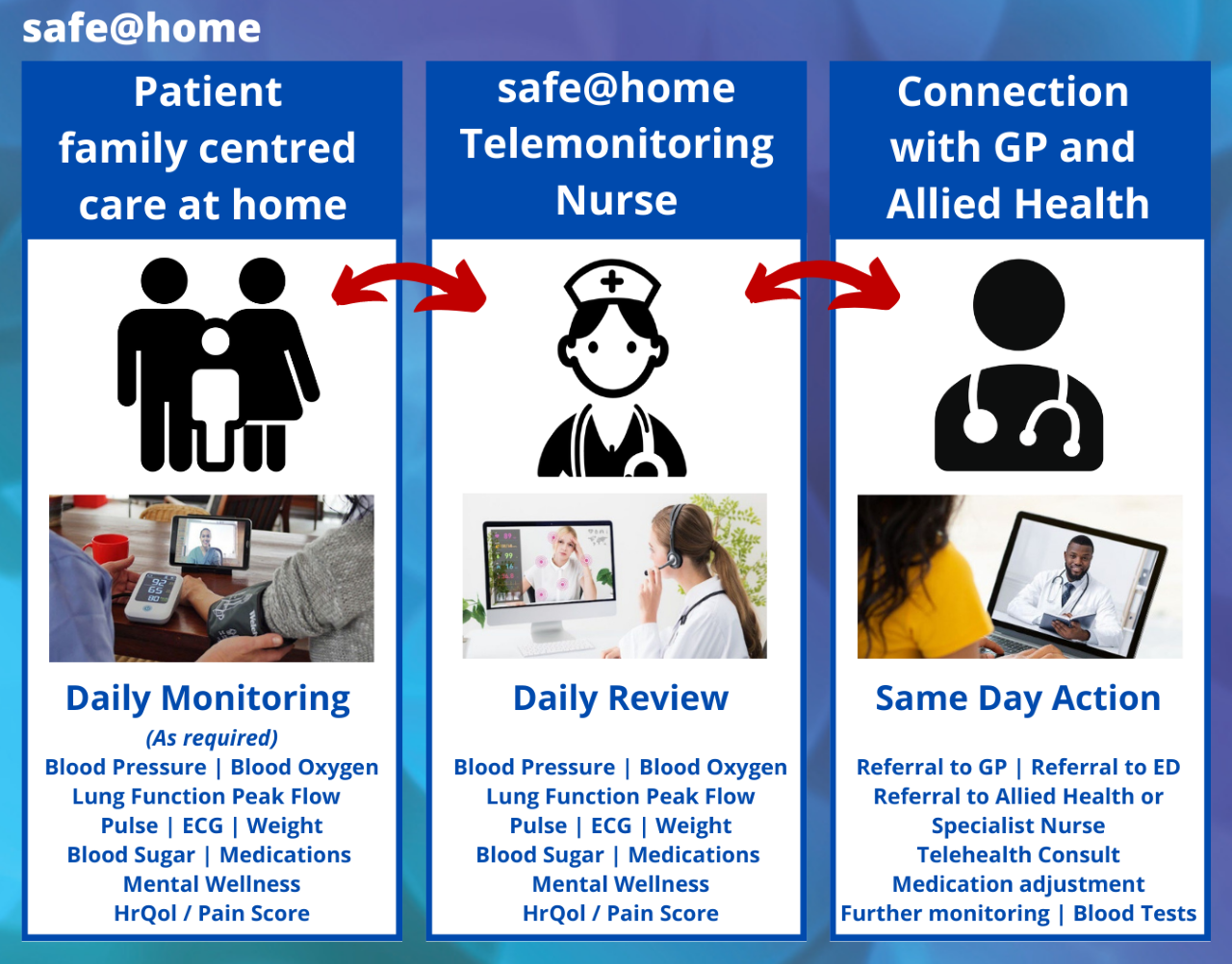
The ‘safe@home’ project will deliver integrated primary care services on a daily or regular basis in the form of fully monitored virtual care and telemonitoring to reduce emergency department and hospital admissions, GP clinic waiting times and ambulance ramping.

The chief investigator – Caring Futures Institute Flinders University Professor Robyn Clark, from the College of Nursing and Health Science – will work with key public health groups across the Adelaide metropolitan area on the new project funded by an almost $1.1 million National Health and Medical Research Council (NHMRC) Partnership Project.
SA Health and other agency involvement includes the Northern Adelaide Local Health Network, the Adelaide Primary Health Network, Australian Telehealth Society, Digital Health SA and Integrated Cardiovascular Clinical Network SA.
Dr John Maddison, the Executive Director of Medical Services at the Northern Adelaide Local Health Network, says the venture is a positive development.
“Embracing technology and linking General Practice with Hospital Care is the best way to keep our patients safe at home, which is better for patients and also helps take the pressure off our emergency departments,” says Dr Maddison.
“With the unrelenting pressure on our healthcare system, we will be focusing on creating a robust primary care framework for people living with high needs, such as heart failure, diabetes, hypertension and chronic obstructive pulmonary disease (COPD),” says Professor Clark, a Professor of Acute Care in Cardiovascular Research with the Caring Futures Institute at Flinders University.
“Along with providing quality care in the home setting, we aim to improve the every day quality of life for these patients by giving them more regular health checks and access to professional help.
“Even more than this monitoring, it is the clinical decisions and actions taken based on information obtained by monitoring that will alter patient wellbeing and outcomes.”
The new project will engage and train clinicians across disciplines (doctors, nurses and allied health) in both hospital and primary care to create a new digital health workforce.
Home telemonitoring and virtual care will involve consumers in their model of care and give them incentive to increase their self-care and self-monitoring to manage their conditions, she says.
It also will be used to develop a business model for other regions to use routine Medicare item numbers for primary care and a framework for scaling into routine care, including refinement of the interfaces with the electronic medical records and patients’ clinics.

Professor Clark also leads the CHAP (Country Heart Attack Prevention) team which is wrapping up a previous $3.2 million NHMRC Partnership Project which built a four-step model of care and clinical pathway for the translation of cardiac rehabilitation and secondary prevention guidelines into practice for rural and remote patients.
The Heart Foundation notes that 1.4 million Australians have a high chance of having a heart attack or stroke in the next five years, with key factors contributing to heart conditions such as high blood pressure and high cholesterol largely preventable.
National Health Week is marked in Australia 1-7 May 2023.

