
Comparisons with international systems and innovations in aged care has identified many opportunities for improvement in Australia, according to researchers at Flinders University.
Flinders University experts from the Rehabilitation, Aged and Extended Care research group and Caring Futures Institute with research partners produced two major reports for the Royal Commission into Aged Care Quality and Safety that examine how aged care is delivered around the world and the types of innovative approaches used.
Flinders University Professor Maria Crotty, senior research fellow Dr Suzanne Dyer, and Professor Anthony Maeder were leads in the reports.
In Research Paper 2: Review of International Systems for Long Term Care of Older People, the authors examine aged care systems in 22 countries.
The report uses available data and assessment of each country’s aged care policies such as financing, accessibility and regulation. The authors note country comparisons are complex and require some judgement.
The authors point to Denmark and Sweden as countries likely to have good quality long-term care systems. Both have government expenditure on long-term care for older people greater than 4% of Gross Domestic Product (based on OECD data), whereas Australia spends around 1.2%.
Both countries fund long term care through local authorities with federal grants and local taxes. Both focus on providing long term care in people’s homes with a moderate proportion of care recipients in residential care institutions.
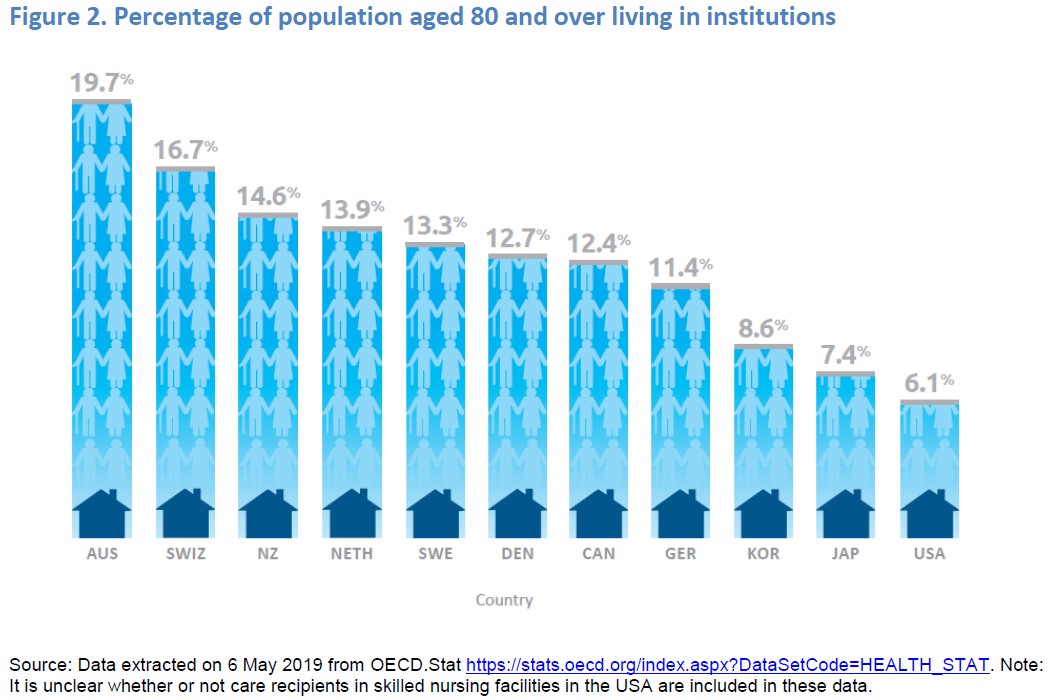
Australia’s spending on long-term care is among the lowest of the countries in the study. A relatively high proportion of Australia’s long-term care recipients are in residential institutions (around 45%) while most other countries support a greater share of their long-term care recipients through home and community care.
Staffing in Australia’s residential institutions appears at the lower end of the range internationally, both for total staffing and nursing.
The level of accessibility to long-term care in Australia was assessed as relatively high, along with Korea, Japan, the Netherlands, New Zealand, Sweden and Switzerland.
Care recipients in these countries have an entitlement to care, are not means tested and can choose the type of provider. These countries vary in other ways, for example Australia scores less well than many for quality of coordination between long-term care and other services including health care.

Australia predominantly regulates aged care quality through a single central agency using an inspection-based approach. Many other nations have multiple levels of responsibility for regulation of quality and many have a decentralised approach.
Some countries, like Japan, Germany and Switzerland have a professionalism based approach. An increasing number of countries use mandatory reporting and provide public data to empower consumer choice and drive improvements in quality.
The report notes the need to think of a care system from the social rather than just economic perspective and highlights some key areas where the authors consider that care for older Australians can be improved:
- Increasing support for home-based care and informal carers – more high-level Home Care Packages and more general leave provisions and financial assistance for informal carers.
- Increased involvement of local or regional authorities in the regulation and monitoring of long-term care services.
- Increased professionalism of the workforce, for example mandatory training or registration of care workers.
- Increased transparency in staffing levels.
- Mandatory reporting and public availability of quality of care indicators, which could include standardised assessments such as the InterRAI or Australian clinical quality registers.
- Better integration with the healthcare system to improve the management of chronic diseases including dementia.
- Stronger focus on rehabilitation and maintaining function to delay and avoid disability.
- Incorporation of principles of human rights in the aged care standards.
In Research Paper 3: Review of Innovative Models of Aged Care, the authors examine approaches to aged care that are not widely available in Australia. The authors identify a range of approaches that could potentially have benefits in Australia including:
- Supports, such as individualised training, for people with dementia living at home and their carers. There is some evidence such supports delay functional decline and reduce depression among carers.
- System navigators or care coordinators who facilitate streamlined access to care for people with dementia or other chronic health conditions.
- Small, domestic residential care homes that maximise the independence of residents and their participation in daily activities. These small homes can be adapted for specialised needs such as people with dementia.
- Respite services provided in settings aligned to people’s backgrounds, such as farm settings for people with dementia living in agricultural areas.
- Training and accreditation practices to increase awareness and availability of culturally appropriate services for people with diverse backgrounds.
- Telehealth communications that enable better access to health and other care services for people less able to travel or who live in remote regions.
- Remote support of independent living through ‘health smart homes’ that use sensors to monitor a person’s health conditions and signs they need assistance.
Both research papers were prepared for the information of the Royal Commission and the public. Any views expressed in them are not necessarily the views of the Commissioners.
To read the research papers, please visit the Royal Commission publications page.
Also link to the recent Flinders Brave Lecture: ‘Handle with care – getting the fundamentals right when caring for older people’ with Professor Alison Kitson. Also ‘What constitutes good quality of care in aged care?’ with Flinders Professor Julie Ratcliffe.


