In more ways than one, research is showing ‘you are what you eat’.
The gastrointestinal tract, which contains 10 times more bacterial cells than the rest of the human body, plays a pivotal role in complex health and wellbeing issues.
Flinders University is conducting several gut research projects through a series of multi-disciplinary collaborations that are exploring this complex issue from several angles – including how the gut ‘communicates’ with the brain.
Only recently has a significant body of evidence been presented that suggests these gut microorganisms, often collectively referred to as the microbiome, can have major effects on human health.
The microbiome has a major role in the development and function of the nervous system through the ‘gut-brain axis’, and a growing understanding of how the microbiome regulates human physiology, including metabolism, immunity and brain function, suggests that a ‘microbiome-gut-brain axis’ may be a more appropriate model for researchers to explore.
The delicate balance between the human microbiome and the development of specific psycho-pathologies is particularly interesting given the ease with which the microbiome can be altered by external factors, such as diet, exercise, exposure to antibiotics or even disrupted sleep patterns.
Flinders University and SA Health and Medical Research Institute (SAHMRI) Associate Professor Stuart Brierley, in collaboration with Professor Nick Spencer, have a National Health and Medical Research Council project grant to study how sensory nerves communicate electrical signals from our internal organs to the brain, and how dysfunction of these sensory pathways leads to improper functioning of these organs, including the bladder and gut.
This research team has also been awarded international funding to study aspects of the microbiome-gut-brain axis affecting human health. This research is funded by a five-year MBIE Research Program grant as part of an international consortium between AgResearch and Fonterra in New Zealand, Flinders University and University College in Ireland.
Flinders University NHMRC Principal Research Fellow Professor Damien Keating is making major advances in understanding how gut-derived hormones control our metabolism, which can regulate obesity and tell our brain when to stop eating.
Professor Keating also has funding from the Australian Research Council and from international pharmaceutical companies. He utilises mouse and human gut tissue to demonstrate how nutrients we eat can affect the release of hormones that send signals to our brain to suppress appetite.
Such a mechanism tells our brain when we’ve had enough to eat, and dysfunction in such systems can cause obesity in humans. He is also establishing the key signals that our microbiome produce, which gut cells receive these signals, and how these cells then control our metabolism.
“These are exciting times, working in a burgeoning scientific field that has direct implications for human health disorders such as psychiatric illness, pain, diabetes and obesity,” says Professor Spencer.
Through the work of these research leaders, Flinders University is leading the way in understanding these complex pathways, with the hope of developing new treatments for major public health problems.
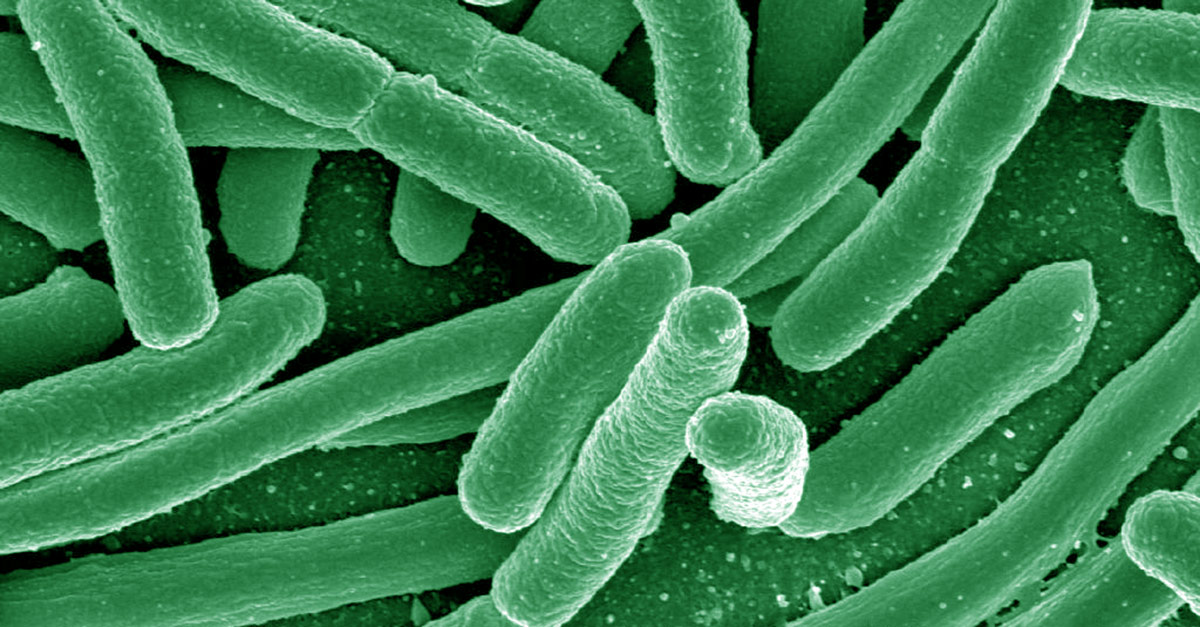
Flinders researcher Dr Geraint Rogers, a molecular microbiologist and microbial ecologist, leads microbiome research at the Infection and Immunity theme at SAHMRI. He gave some background in an interview with ABC TV on the Weekend Breakfast program.
“Characterising the metabolic products of the intestinal microbiota is essential in understanding how they influence a person’s health,” Dr Rogers told the American Society for Microbiology last year. “These compounds can modulate a person’s immune regulation, central nervous system function and metabolism.”
“Analysing antibiotic-induced disturbances in the gut microbiota and its corresponding metabolome can therefore provide insight into both the acute and chronic effects of antibiotics, and may give a functional understanding of the development of any associated health conditions.”

