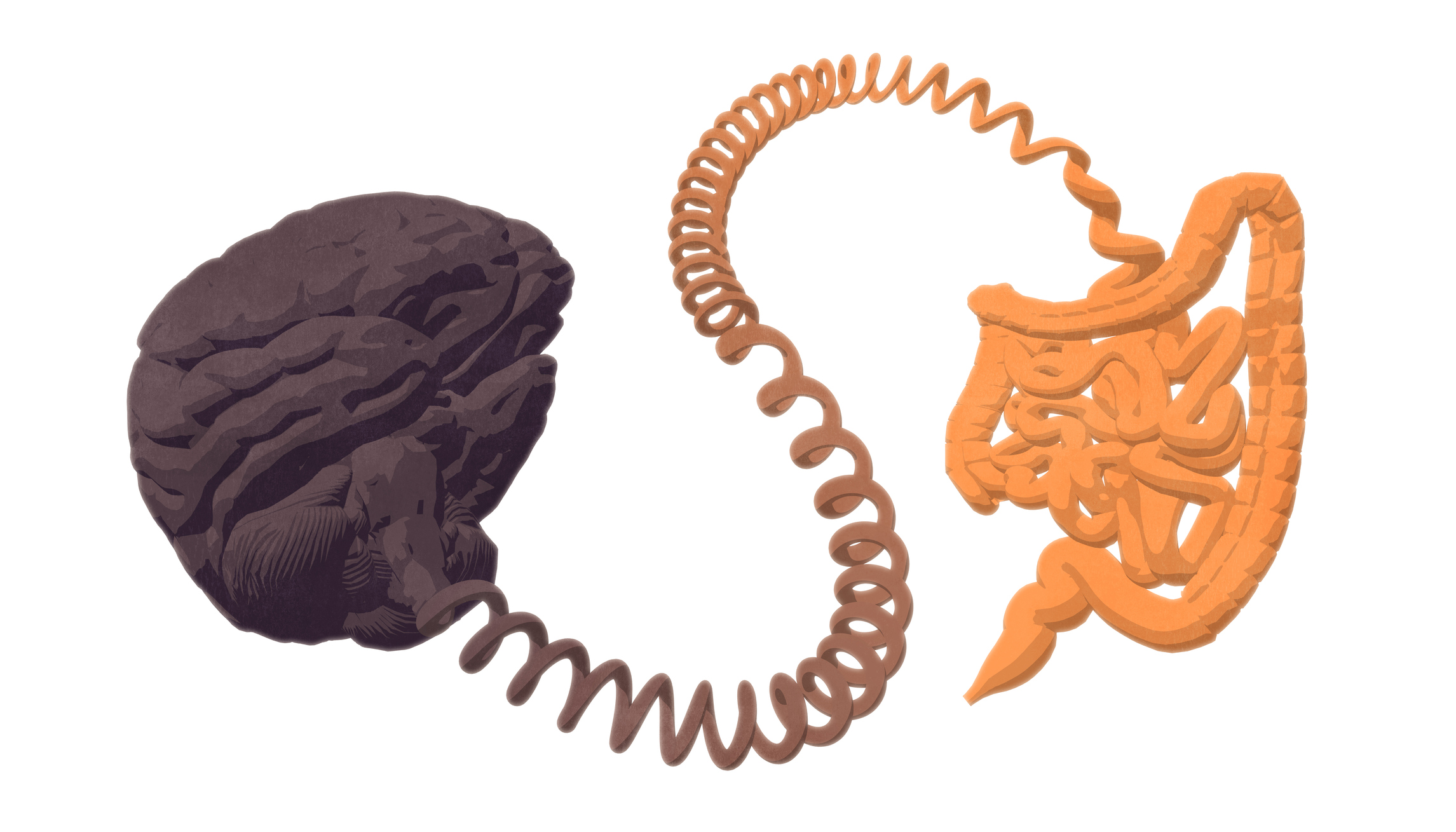
Scientists at Flinders University have, for the first time, identified a specific type of sensory nerve ending in the gut and how these may ‘talk’ to the spinal cord, communicating pain or discomfort to the brain.
This discovery is set to inform the development of new medications to treat problems associated with gut-to-brain communication, paving the way for targeted treatments to mitigate related dysfunction.
While our understanding of the gut’s neurosensory abilities has grown rapidly in recent years, two of the great mysteries have been where and how the different types of sensory nerve endings in the gut lie, and how they are activated.
An important step in answering these questions has been made possible through the development of new techniques by Professor Nick Spencer’s Visceral Neurophysiology laboratory at Flinders University in South Australia.
“We know that many disorders of the brain and gut are associated with each other, so unravelling their connection is critical to developing targeted, efficient treatments for what can be debilitating conditions like irritable bowel syndrome, chronic constipation or ulcerative colitis,” Professor Spencer says.
Professor Spencer’s research revealed an extraordinarily complex array of nerve endings that are located over multiple layers of tissues in the lower colon.
“Our study identified the two classes of neurons involved and their location in a range layers in the colon including muscle and mucus membranes, which are potentially capable of detecting sensory stimuli.”
His research forms one of many studies underway at Flinders University’s five neurogastroenterology laboratories, which are contributing to the growing bank of global knowledge on the gut’s interaction with the brain, including its impact on higher cognitive function.
This research was supported by grants from the Australian Research Council (ARC) and the National Health and Medical Research Council (NHMRC).
The paper was published in the Journal of Comparative Neurology.

