Australian researchers have identified a link between itchy skin and gut pain, caused by identical receptors signalling the nervous system.
This is big news for Irritable Bowel Syndrome (IBS) patients, who make up 11 percent of the world’s population, with the fight against chronic pain taking a major step forward. It is hoped the identification of these receptors in the nervous system may see the development of effective treatments.
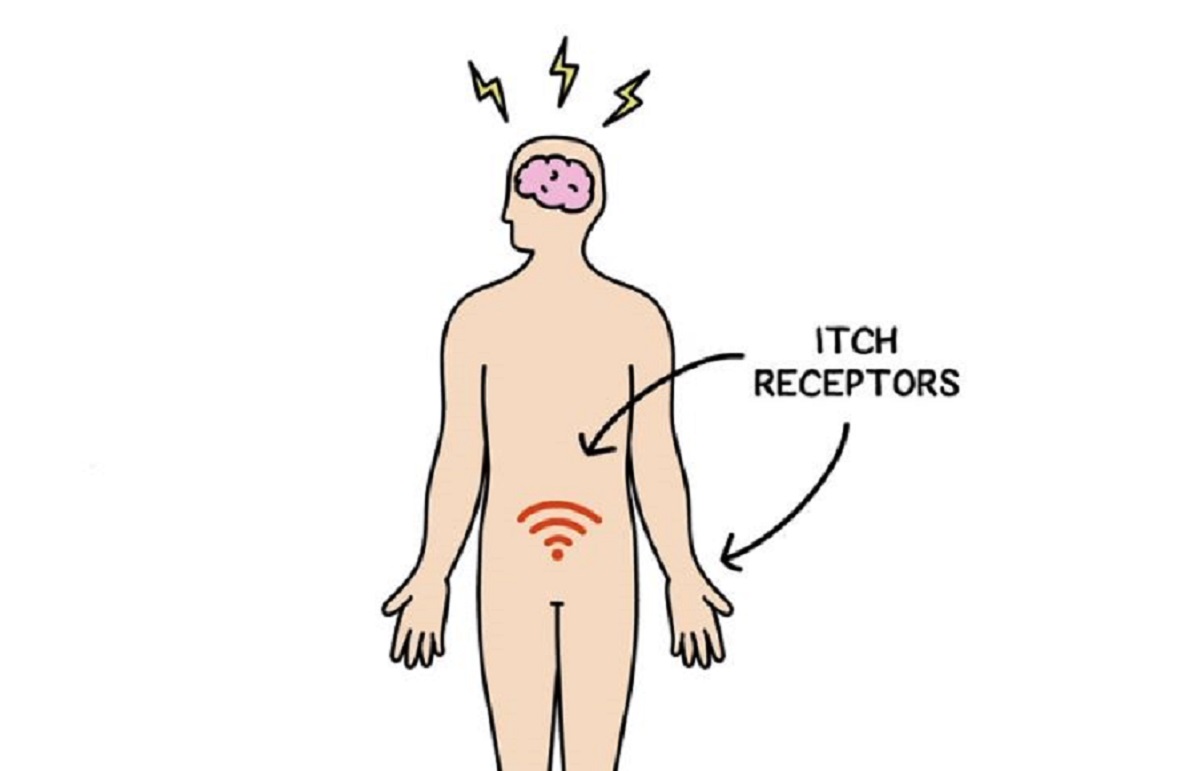
Flinders University researchers at SAHMRI discovered receptors that cause itchy skin also exist in the human gut. These activated neurons, which result in IBS patients experiencing chronic gut pain – or a seriously painful ‘gut itch.’
In millions of Australians with IBS, it seems these ‘itch’ receptors might be more numerous than in healthy people. This means more neurons are activated, causing the sensation of pain.
NHMRC and Matthew Flinders Research Fellow in Gastrointestinal Neuroscience, Professor Stuart Brierley, says these gut itch receptors could offer a new way of targeting the underlying cause of gut pain, rather than using traditional drugs (like opioids), which don’t fix the problem immediately.
“We found receptors that bring about an itchy feeling on skin also do the same in the gut, so these patients are essentially suffering from a ‘gut itch’,” Professor Brierley says.
“We’ve translated these results to human tissue tests and now hope to help create a treatment where people can take an oral medication for IBS.
“Patients with IBS suffer from chronic abdominal pain and experience a ‘rewiring’ of their nervous system so they feel pain when they shouldn’t – we decided to ask important questions about how nerves in the gut are activated to cause pain in order to seek out potential solutions.”
Professor Brierley, also the Director of the Visceral Pain Research Group at SAHMRI, says pain experienced by IBS sufferers takes place when itch receptors are coupled with what’s known as the ‘wasabi receptor’ in the nervous system, which normally causes a reaction in people consuming wasabi, the Japanese condiment.
“If you think about what happens when you eat wasabi, it activates a receptor on the nerves and sends a pain signal – that’s exactly what’s happening within their gut as they experience an itch.
“Having shown these mechanisms contribute to chronic gut pain, we can now work out ways to block these receptors and thereby stop the ‘gut itch’ signal travelling from the gut to the brain. This will be a far better solution than the problems currently presented by opioid treatments”.
Professor Brierley’s research was funded by the National Health and Medical Research Council in Australia. View the paper: https://insight.jci.org/articles/view/131712

