Despite increased education, Australians continue to have a poor understanding of the age-related decline in natural and IVF-assisted conception, potentially explaining why many delay starting a family.
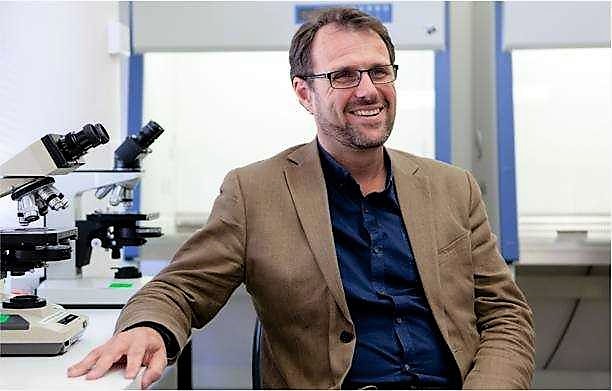
A greater uptake of ovarian reserve screening may help identify individuals at increased risk of premature diminished fertility, according to Professor Kelton Tremellen, Professor of Reproductive Medicine at Flinders University.
He says that such screening may prompt women identified as having low ovarian reserve to bring forward their plans for natural conception or possibly undertake fertility preservation (oocyte freezing) – but he is alarmed that community knowledge about ovarian reserve screening is scant.
This issue is explored in a paper, “Australians’ understanding of the decline in fertility with increasing age and attitudes towards ovarian reserve screening” (2018), by Flinders researchers Alisha Evans, Sheryl de Lacey and Kelton Tremellen, in the Australian Journal of Primary Health (CSIRO Publishing, doi.org/10.1071/PY18040).
Despite Australia’s four-decade trend towards older parenthood, men and women consistently overestimate natural and IVF-assisted fertility with increasing age, which may explain why many feel comfortable delaying starting a family until after age 30 years, a stage when fertility is already compromised.
The aim of this study was to determine Australians’ understanding of the decline in fertility with age, social determinants that influence their decision to start a family and attitudes towards ovarian reserve screening as a tool allowing personalised reproductive life planning.
The Flinders University researchers conducted an online survey of 383 childless Australian men and women, aged 18–45 years, in 2016.
Both sexes overestimated natural and in vitro fertilization (IVF)-assisted fertility potential with increasing age, with the magnitude of overestimation being more pronounced for men and IVF treatment compared with natural conception.
“People generally overestimate female fertility and plan to delay having a family without anticipating difficulty conceiving,” says Professor Tremellen, suggesting the usefulness of the widely offered Anti-Müllerian hormone (AMH) test to give one indication of fertility.
“We suggest that addition of AMH ovarian reserve screening to routine tests, such as cervical cancer screening, for women without children who are aged more than 30 years, would improve reproductive awareness and may enhance their chances of parenthood by identifying women with accelerated ‘ageing’ of their ovaries,” he says.
Other measures can also keep individuals informed of their fertility.
The study identified that the primary social determinants for starting a family were availability of a suitable partner and attainment of educational and career goals, rather than the availability of affordable childcare and parental leave.
As education and career advancement are positive initiatives that should not be reversed, there appears to be little that governments can do in relation to policy that may help drive down the average age of starting a family.
Poor understanding of the significant decline in reproductive potential with increasing age suggests that educational campaigns have so far been ineffective, and cast doubt on whether further education campaigns are the best approach to reverse the trend of delayed child-rearing.
The study was the first to assess Australians’ knowledge of and response to AMH-based OR screening, with screening being considered a useful reproductive planning tool by the majority of Australian women but less so for men.