Much-needed solutions to chronic pain, bowel cancer, drug delivery and improved childhood vaccinations are a step closer to reality thanks to newly funded Flinders University research.
This follows Australia’s National Health and Medical Research Council today awarding $526 million for research across Australia, with Flinders University receiving more than $5.9 million in eight direct project grants, and lending support to a further two projects.
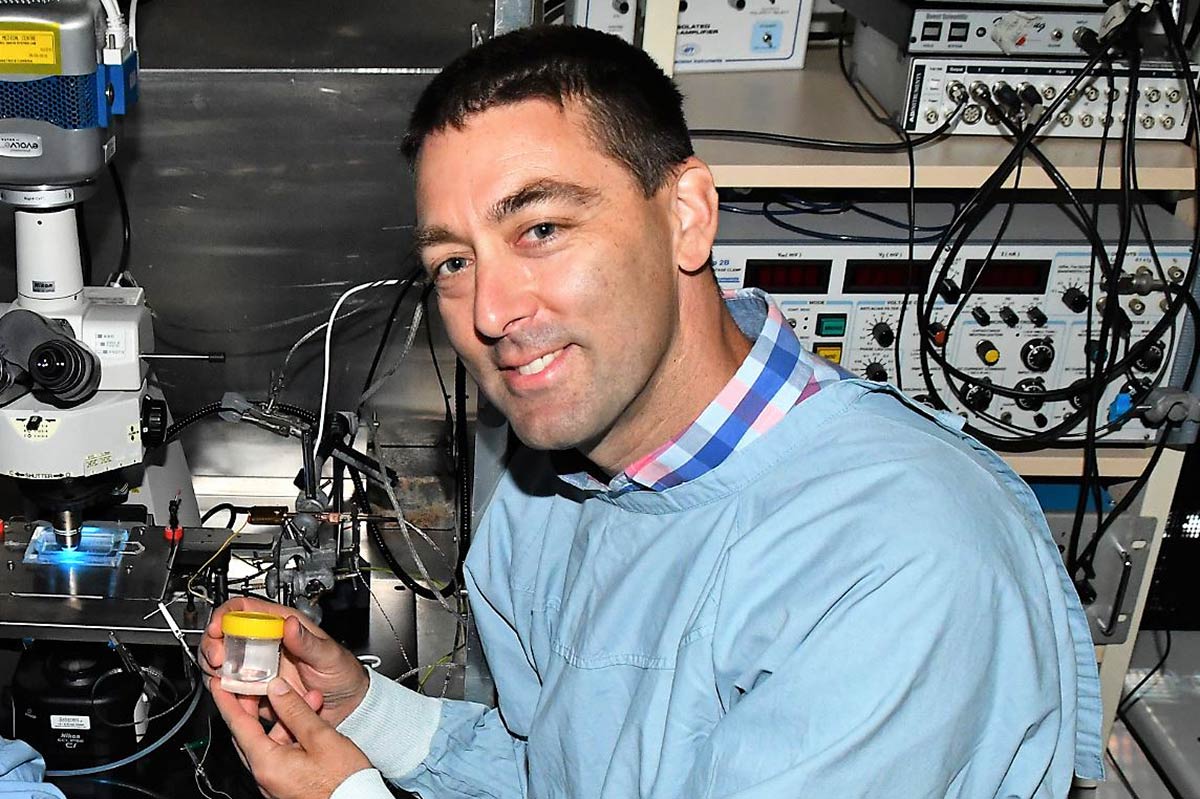
Professor Nicholas Spencer has secured funding to lead two projects to find the cause and cure for abdominal gut pain.
“There is a desperate need for alternative therapies or techniques to suppress chronic pain instead of using opioids for pain relief,” says lead investigator Professor Nicholas Spencer, from the Flinders College of Medicine and Public Health.
“Our Visceral Neurophysiology Laboratory team is using a novel approach known as optogenetics – the use of light to control cells in living tissue – to target the sensory nerve cells in the intestines. We’re finding new ways to use light to manage chronic conditions such as irritable bowel syndrome and constipation without the negative side-effects of regular treatments.”

New research into whether antibiotic exposure in early life can impair immune responses to infant vaccinations, led by Flinders Associate Professor David Lynn, will move to human trials after new published preclinical work showed that this is the case in mice.
Professor Lynn says effective vaccine responses are essential to childhood and community health globally, and the data in mice suggests that antibiotics could compromise the microbes that may support optimal immune responses to vaccines.
“We will investigate how the collection of microbes in the infant intestine – the gut microbiota – can influence vaccine responses in infants,” says Professor Lynn, who is based at Flinders and the SA Health and Medical Research Institute (SAHMRI).
Personalised detection of bowel cancer, and a promising new method to more effectively deliver drugs with fewer side effects are amongst other key projects to be funded.
“The latest round of NHMRC project grants highlights Flinders University’s long-running research strengths in producing more effective and safe drugs, vaccines and diagnostic tests for major diseases including cancer, diabetes, and even obesity,” says Flinders University Deputy Vice-Chancellor (Research) Professor Robert Saint.
“The funding is vital to deliver outcomes urgently needed for better treatments and health in both advanced and developing countries,” Professor Saint says.
“It has been an outstanding year for major federal research funding at Flinders, and the latest grants will help guarantee real-world outcomes from the world-class research efforts at Flinders University,” Professor Saint says.
Further details of the Flinders projects to commence in 2019 are:
- ‘Silencing visceral pain pathways using novel optogenetic techniques in vivo’. Led by Professor Nicholas Spencer and co-investigators Associate Professor Stuart Brierley (Flinders and SAHMRI), Associate Professor Vladimir Zagorodnyuk (Flinders) and Dr Andrea Harrington (University of Adelaide). $922,848.
- ‘Wireless optogenetic induction of gastrointestinal transit in conscious mice’ led by Professor Nick Spencer and co-investigator Associate Professor Hongzhen Hu (Washington University Missouri, USA). $788,589.
- ‘How does the microbiota modulate vaccine responses in human infants: A systems vaccinology approach.’ Led by Associate Professor David Lynn (Flinders, SAHMRI and EMBL Australia) and co-investigators Professor Geraint Rogers (Flinders and SAHMRI), Professor Helen Marshall (University Adelaide) and Dr Damon Tumes (SAHMRI). $858,033.
- ‘FIT for purpose: personalised surveillance colonoscopy for people at increased risk of colorectal cancer’ led by Dr Erin Symonds (Flinders and SA Health) and co-investigators Emeritus Professor Graeme Young (Flinders), Professor Carlene Wilson (Flinders and Olivia Newton John Cancer Research Institute, Melbourne), Dr Peter Bampton (Flinders and SA Health) and Professor Ernst Kuipers (Erasmus University Medical Centre, Netherlands). $880,237.
- ‘ADMExosomes: A new paradigm for tracking variability in drug exposure’ led by Dr Andrew Rowland and Flinders co-investigators Professor Michael Sorich (Flinders) and Emeritus Professor Peter Mackenzie. $731,812.
- ‘Targeting proglucagon cells in the human gut to treat diabetes and obesity’ led by Professor Damien Keating and co-investigators Associate Professor Richard Young (Adelaide University), Professor Jens Holst (University of Copenhagen, Denmark) and Professor Filip Knop (Copenhagen Uni). $712,083.
- ‘Novel feedback inhibition of AMPK by mTORC1 controls cell proliferation under stress’ led by Associate Professor Janni Petersen (Flinders) and co-investigator Associate Professor Jon Oakhill (St Vincent’s Institute of Medical Research, Melbourne). $625,788.
- ‘Colonic dysmotility is a significant aetiological factor in faecal incontinence’ led by Associate Professor Philip Dinning (FMC / Flinders Uni), Professor Simon Brookes (Flinders), Dr Lukasz Wiklendt (Flinders), Professor David Wattchow (FMC / Flinders) and Professor Marcello Costa (Flinders Uni). $422,324.
Other Flinders University College of Medicine and Public Health scientists Professor Judith Dwyer and Professor Briony Forbes are co-collaborators in two other major projects respectively led by the University of SA and Florey Institute of Neuroscience and Mental Health in Melbourne.

The latest round of NHMRC funding includes $86 million for cancer research, more than $61 million for cardiovascular disease investigations, more than $41 million for mental health research, $29 million for diabetes research and $28 million for obesity research.

